The science of vaccination
Audio: Listen to audio clip.
BitDepth#1305
IT MIGHT be disturbing to know, but at the best of times, in the flush of good health, our bodies are teeming with germs and bacteria, most of which are essential to maintaining the balance that's necessary for human health.
Most of your immune system’s time is spent dealing with unwanted germs, parasites, fungus and viruses, from the common cold to covid19. These unwelcome invaders are collectively called pathogens, and the body is constantly looking out for a protein in their mass called antigens, which trigger the formation of antibodies, your immune system's response to the threat.
All this happens without anyone being more aware of it than the muscles that make the heart beat or lungs expand.
Most uncompromised immune systems are full of information gathered throughout your life about the pathogens you have encountered, because the ability to identify and act on new antigens is built into the memory cells of the body.
But it wasn't Panadol or cough syrup – which treat the symptoms of illness – that responded to the pathogens. The work was done by your antibodies, learning as they went along about how to deal with new variants of such regular party-crashers as a new minor flu or cold.
There are more than 200 virus families that are known to cause the common cold, and chances are you haven't been exposed to even half of them yet.
Which brings us to covid19, which earned the name "the novel coronavirus" when it was discovered in 2019.
When this highly infectious disease began blazing through the population of Wuhan in China, nobody knew anything about it. Eighteen months later, having invested hundreds of thousands of man-hours' worth of study, there is still a lot we don't know.
In 2003, the outbreak of Severe Acute Respiratory Syndrome (SARS) in China began the research into deadly, airborne, highly infectious diseases. Officially, covid19 is known as SARS-CoV-2.
AstraZeneca and Johnson & Johnson vaccines use adenovirus-vectored technology. The AstraZeneca serum piggybacks a gene from covid19 on a harmless common-cold virus to trigger antibody production.
Pfizer-BioNTech and Moderna use mRNA technology, which uses a genetic code that tricks the body into producing antibodies.
Vaccines trigger symptoms as the body responds to phantom illnesses, but the payoff is an immune system that's primed to respond to a real covid19 infection.
Vaccination is necessary and sensible, but it won't be a magic bullet. The defence against covid19 will demand multiple strategies, sustained until the virus joins smallpox and polio in medical history.
Neither of those viruses mutated as easily as covid19 and inspired a global vaccination drive to eradicate them.
Even so, Jonas Salk's polio vaccine was introduced in 1955 and preventive vaccination continues to this day.
Edward Jenner's smallpox immunisation was first administered in 1796, but it wasn't until 1980 that the variola virus was considered eradicated.
The next challenge will be dealing with variants, the significant mutations of covid19, particularly those that emerged from Indian (B.1.617) and South African (B.1.351) pandemic spread. Variants also make it difficult to predict when herd immunity will become a reality with covid19, because neutralising their spread with vaccines is difficult.
Back to normal, even with vaccination, may include masks and physical distancing, for those who can't or won't be vaccinated for medical or philosophical reasons, for some time yet.
These variants point to a long battle with covid19 and the possibility that regular booster vaccination and a variation of existing restrictions will be part of our daily lives for months, if not years, to come.
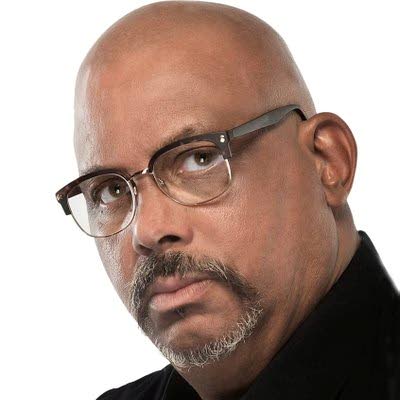
Mark Lyndersay is the editor of technewstt.com. An expanded version of this column can be found there

Comments
"The science of vaccination"