The 2020 HIV/Aids mission

Human mobility has increased in Latin America and the Caribbean and if countries hope to maintain their projection to eliminate the spread of the HIV/Aids by 2030, it would be a good public health practice to give migrants treatment.
UNAids regional director for Latin America and the Caribbean Dr César Nunez said governments should welcome migrants, because they bring more good than bad.
He said in many cases people in mobile populations are ill-treated and even subjected to sexual trafficking, and there should be policies addressing the need to protect them which should include the availability of HIV treatment, because it would not only benefit the migrants but protect the host country from transmission.
Part of the 2016 HIV declaration to eliminate the spread of the virus by 2030 is a commitment to fast-track the response. The 90-90-90 target indicated that by 2020, 90 per cent of those infected should know their status; 90 per cent of that number should be put on antiretroviral drugs; and 90 per cent of those should have their viral loads suppressed to an undetectable level. If the virus cannot be detected, it cannot be transmitted.
Nunez, who was in TT for the Second Regional Seminar for Parliaments of the Caribbean on December 5, explained that every two years UNAids invites governments to share data in a workshop to take stock of what has been done so far. The next workshop for estimates will take place in 2021, although it is expected that countries supply 2019 data by March 31, 2020.
He said governments have the tools for an effective prevention and treatment plan, as well as to address stigmatisation and discrimination. He believes TT is on track to being close to meeting its goals, given the 2016 and 2017 numbers.
However, he hopes TT will increase its efforts, and suggests increasing the number of testing sites and the availability of drugs.
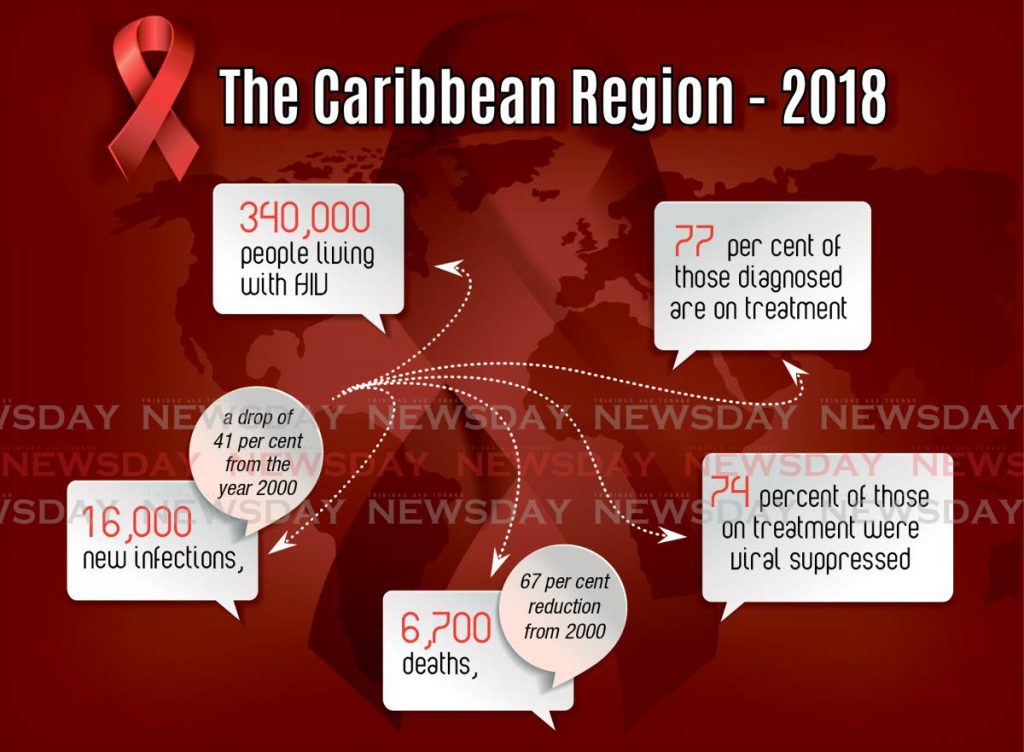
In the Caribbean region, he said, there are 340,000 people living with HIV. In 2018 there were 16,000 new infections, a 41 per cent drop from 2000. There were also 6,700 deaths, a 67 per cent reduction from 2000. He added that 77 per cent of those diagnosed are on treatment and 74 per cent of those being treated were virally suppressed. He added that in nearly all Caribbean countries, viral suppression among men is lower than among women, so it is necessary to improve services to men.
“If treatment is given correctly, without interruptions, we would also add a protection effect to people who may engage in sexual relationships with somebody who is receiving treatment.”
He feels the progress towards the 2020 target has come to a plateau, because there are still new cases despite the number of people on treatment. He said UNAids needs Caribbean countries to reach out to those living with HIV, including those who do not know they are infected.
One challenge is late diagnosis. Five out of 12 countries reporting data showed half of newly diagnosed cases present with advanced HIV.
“So people are not coming to be tested because they have been informed, or because they attended a particular session. People come when they feel ill, if at all. And when they come, more than 50 per cent of the cases already have advanced signs of the disease.”
Therefore, he said, more aggressive strategies are needed and suggested several.
The first is self-testing, which he compared to a home pregnancy test that is both specific and sensitive enough to be accurate. He said the test is already being used in Brazil and he hopes other countries will follow.
In the past, Nunez said, people believed finding out they had tested positive was too difficult to face without some sort of support. But with the effective treatment available, most people recognise that HIV is not a death sentence. In this way, after a positive result, people can get a more sophisticated analysis and start treatment immediately.
“Treatment would not only be good for them, but from a public health point of view, it will be good for the country, because it will be able to prevent new infections from this particular person, since they will become undetectable or virally suppressed.”
Another strategy, he said, is for every woman who goes for antenatal care during her first trimester to be tested for HIV. In this way she herself can receive treatment as well as
prevent her baby from being born with the virus.
“I believe the Caribbean has done a very good job at the elimination of mother-to-child transmission. Cuba was the first country in the world to have eliminated paediatric HIV. They were certified by WHO, UNICEF and UNAids and every two years they need to recertify, because if they lower their guard, HIV can resurge.”
Since Cuba, six more territories in the Caribbean – Anguilla, Antigua and Barbuda, Bermuda, Cayman Islands, Montserrat, and St Kitts and Nevis – have been certified. And although they have to maintain the certification, he believes they will do so and that more Caribbean countries will gain certification.
He said it is also public health good practice to do index testing. This means if someone tests positive, every member of the household should be invited to be tested as well.
“It doesn’t matter the age or the gender, every member of that household should be tested. We have found when you do that, we identify more members of the household already living with HIV.”
Nunez explained, “All of the measures are meant to corner HIV and stop it, because if we keep on getting new infections, it will be costly. Even if you buy the least expensive treatment, 16,000 times $100 per year is a lot of money...The fiscal space available to make sure that TT is the leader on those promises (of the 2030 agenda) is limited.”
Nunez said treatment used to be several pills which cost US$10,000 per person per year. Now a person can take one pill a day which costs about US$80 per person per year. Therefore, to ensure the sustainability of the programmes and contribute to the progress of countries, it is necessary to reduce treatment costs through prevention.
He also recognises the role of communities, including women, indigenous, and sexual diversity groups. He said their leadership and advocacy ensures the response remains relevant and grounded, and that people remain at the centre of the response, rather than other issues. At a time when reduced funding threatens treatment programmes, he said, communities ensure HIV remains on the political agenda, that human rights are addressed, and that decision-makers are held accountable for their HIV response.

Comments
"The 2020 HIV/Aids mission"