Screening for breast cancer
Almost all women of a certain age have been taught why and how to do a breast self-examination. It’s simple really: at least once a month – perhaps a few days after your period when your breasts are less swollen and tender – get into the habit of looking at your breasts critically in a mirror for changes in shape or unusual skin deformities. Then, lie back or stand and probe your breasts in a circular pattern using the pads of your fingers in a firm, smooth touch to look for unusual lumps or bumps. (See page 14)
Most women (yes, men can get breast cancer too) are advised to do a self-exam from the time they turn 20. According to breastcancer.org, about one in eight women in the United States (12 per cent) will develop breast cancer in their lifetime. The risk increases as women get older. (See box).
Getting screened
There’s no hard and fast rule when screening for breast cancer should begin because there are several factors that can determine risk – including family history, breast tissue density, age and other pre-existing conditions. As women get older, annual or bi-annual mammograms and ultrasounds are recommended, in addition to regular screening.
Dr Sasha Farrier, family doctor at the Venus Clinic in St Augustine, broke down the process of what to expect when going for a consultation. The process starts with a conversation about family history.
“In medicine, screening for a disease means looking for a disease that isn't giving any signs or symptoms. The point of screening is to try to pick up a disease in its early stages, before it gets time to do damage, and when treatment would generally be the most effective. Therefore, breast cancer screening is generally done as part of a woman's checkup, who hasn't had any symptoms,” Dr Farrier said.
Some of the questions the doctor will ask include:
- Your age
- Whether you've ever had any breast issues in the past
- Family history of breast and other certain types of cancer
- If you've ever had certain other types of cancers
- Your medical history
- Whether you've had any children and if they were breastfed
- Whether you've ever been on any hormonal treatment and for how long
- If you smoke cigarettes or drink alcohol
- What medications you may be taking
- If you perform routine self-examinations (not necessarily full breast exams)
- Results of your last screening
Next comes the examination, which is non-invasive and usually painless, however mild tenderness can occur.
“If you are someone who has tender breasts around your period, it is recommended not to schedule your check up around this time to avoid undue pain,” she said.
Sometimes the patient may request (or the doctor may suggest) a chaperone to help make the process more comfortable, especially because of how intimate the examination can be, she added. The examination itself is a bit like a more specialised self-exam.
“Your doctor will observe and palpate (examine by touching with mild pressure) the breasts and underneath the arms and just above the collarbone. Your doctor may ask you to do different things during the examination, for example sit up, lie down, or press the hands on the hips,” said Dr Farrier.
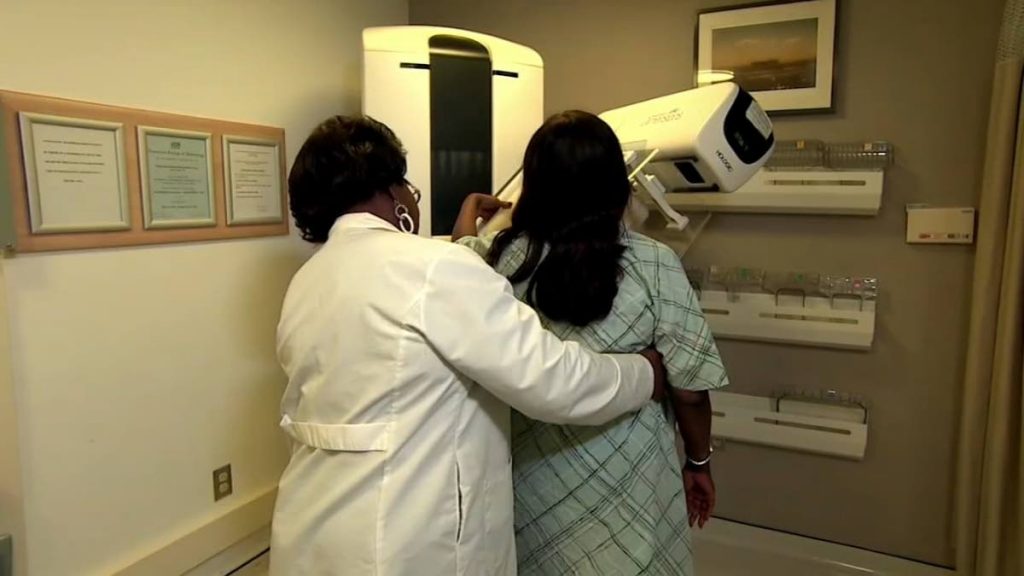
The last step is imaging.
“There are different types of imaging that can be used, but by far the two most common types in screening are the breast ultrasound and mammogram,” she said. A breast ultrasound is very similar to ultrasound done on pregnant women – using an ultrasound probe and gel. Usually there is no pain associated. A mammogram is a test using x-rays to image the breasts. The breasts may be positioned between plates, which apply slight pressure during imaging. Because of this, the mammogram may cause some pain or tenderness in some people. Again, if you have tender breasts before or around your period, it is best to schedule your mammogram at another time to avoid undue pain, Dr Farrier added.
“Your doctor will take many factors into consideration before choosing which test to send you for. In fact, many times, you may be asked to do both. This is because certain things show up better on one imaging over another. There are other forms of imaging available, like an MRI, but because of the increased cost this is usually reserved for special cases.”
Looking for a lump
Mammograms and ultrasounds are usually recommended as women get older and the risk increases – usually from age 50 – but depending on circumstance, doctors may recommend such screening to start from late 30s.
Another factor is the type of breast tissue. Breasts comprise primarily dense and non-dense tissue. Non-dense tissue is primarily fatty tissue. Dense tissue includes connective tissue (kind of like plastic wrap, holding things together), milk glands and milk ducts. Some women have more fibrous – or denser – breasts. Sometimes, especially on women with more fibrous breast tissue, mammograms may be distorted or not clearly pick up abnormalities. That’s usually when the doctor might ask for an ultrasound as a back-up, Dr Farrier said.
“Breast don’t have muscles – chest muscles are underneath – but the breast itself is made up of this dense and non-dense tissue, the proportions of which vary for each woman.”
That’s why it’s important to do a breast examination – to be able to determine for certain the cause of any unusual anomalies.
“Even if you don’t do a full clinical breast exam, we recommend that patients at least feel their breasts from time to time to get an idea of their bodies. When you familiarise yourself with the way your breasts feel, you can more easily determine if there’s any significant change,” she said. “Be aware of how your own breast feels. And of course, try to keep yourself healthy – exercise regularly, follow a balanced diet and don’t smoke.”


Comments
"Screening for breast cancer"