Coronavirus pandemic brings telemedicine to the fore

A week ago, when Kedon Greenidge discovered a rash near his hairline that refused to go away on its own, he counted himself lucky to find a specialist doctor who offered him an online consultation.
Greenidge, 33, said he was immediately impressed with both the technology and Dr Naomi Dolly’s virtual bedside manners.
But more than the time or money the online assessment saved him, what he valued most was getting professional advice minus the risks associated with leaving his home during the coronavirus outbreak.
It’s been two months since the country confirmed its first case. Yet so much about the impact of covid19 on TT’s healthcare system remains unknown: the precise nature of the care afforded to patients who are hospitalised after testing positive for covid19. What happens if there is a spike in cases that overwhelms primary facilities. How a prolonged lockdown might affect access to healthcare not related to the coronavirus.
Even so, there appears to be growing consensus around one thing: the coronavirus has accelerated the need for telemedicine solutions and it’s already remaking the way doctors like Naomi Dolly deliver healthcare.
“I’ve been trying to convert a lot of my patients to telemedicine, which is what the recommendation is internationally: to see your patients remotely,” said Dolly. “But a lot of people don’t even understand what it is. We’re still in an era where we want to see the doctor in person.”
In-person visits may be all well and good under normal circumstances. But given the highly contagious nature of the coronavirus, both patients and the healthcare professionals attending to them risk becoming infected even at the doctor’s office.
Telemedicine, according to Dolly, is nothing more than using technology to deliver healthcare remotely, making it a safer alternative to in-person visits during covid19.
In recent weeks, she has been working to change patient attitudes at her private practice in Woodbrook where she treats diseases affecting the skin, hair and nails in both children and adults.
That meant limiting the number of walk-ins, educating her patients on how telemedicine would work, and then setting up remote consultations for the vast majority of them.
Dolly relies on a mix of apps and tools including Klara, a purpose-built telemedicine app which provides her with a secure communication platform to connect with her regular patients, and more recently, Skype or FaceTime for initial enquiries.
To reduce the amount of time her patients spend on the road, she emails or faxes prescriptions directly to pharmacies like SuperPharm on their behalf.
When his consultation was over, Greenidge told Business Day he had the option to pay his bill via direct deposit or online through the firm’s website.
Dolly isn’t alone in this digital approach to patient care.

Gregory Arneaud of ISD Health Solutions, which treats a range of sleep disorders at offices in Port of Spain and San Fernando, said he’s been practising telemedicine in TT for eight years.
As he sees it, the covid19 crisis is the ideal catalyst for prioritising telemedicine, not least because, by reducing the need for people to leave their homes, it helps to slow the pathogen’s spread.
“Doctors are trying to minimise patients who are not critical from coming in to the office,” Arneaud said. “At the same time, patients being kept at home would like to be able to have some kind of access to medical advice, so it’s a perfect time for this.”
It helped that when he first started ISD Health sleep medicine was a niche area with strong demand.
But that notwithstanding, Arneaud says patient response to ISD Health’s telemedicine tools – including a range of digitally-enabled sleep devices – has been uniformly positive.
“As patients were testing with these devices in the convenience of their own homes – obviously, people sleep better in their own homes – we would send that information via the internet to the United States and the physician would then review the data that was collected from the testing device and then provide documentation and a plan of treatment.”
None of the technology is fly-by-night in the least.
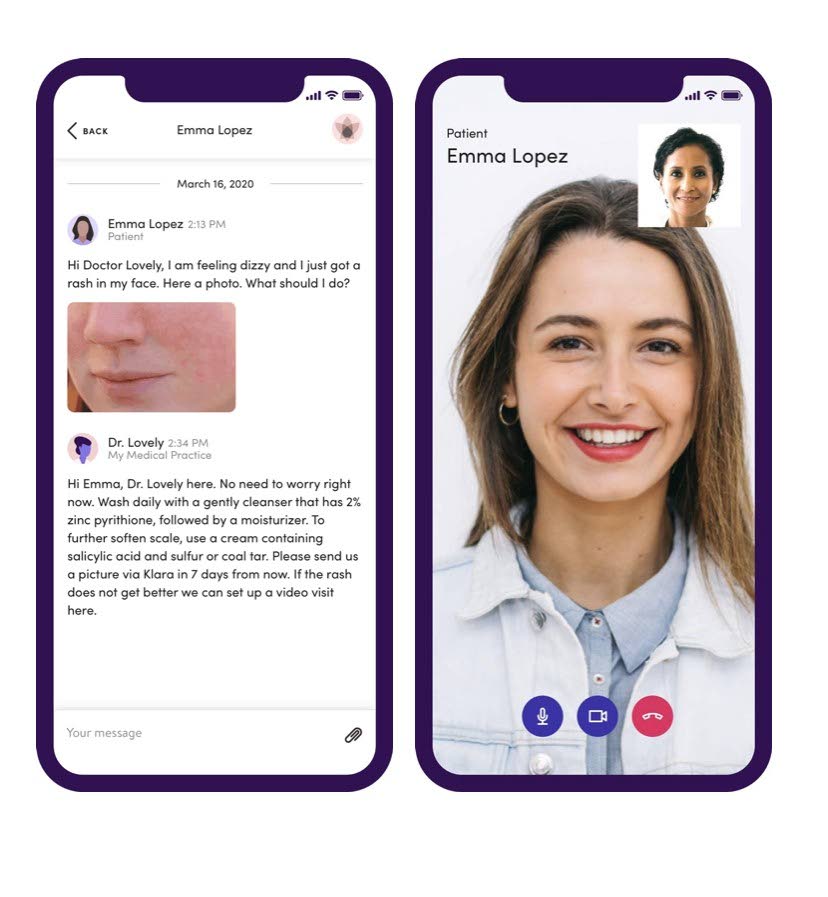
(Photo via klara.com) -
ISD Health’s sleep devices – like the Klara application Dolly uses in her private practice – are compliant with the Health Insurance Portability and Accountability Act (HIPAA), a US law viewed worldwide as the gold standard for ensuring privacy standards and protecting patients' medical records and other health information.
Both Dolly and Arneaud have adopted the HIPAA standard despite the fact that local regulations around telemedicine are virtually nonexistent.
That’s something president of the TT Medical Board Dr Varma Deyalsingh expects to change post-covid19.
“In Trinidad, with this covid19 crisis, it has certainly put us in a position where we have to develop telemedicine,” said Dr Deyalsingh, “And there are protocols already being put in place by some organisations to support it.”
Among those organisations, Sagicor, one of the country’s leading insurers, appears to have taken the lead.
One week ago, the company announced it would extend its healthcare coverage during the covid19 pandemic for patients who consulted their doctors virtually and honour claims related to general practitioner consultations, specialist consultations, one-on-one psychiatrist/psychologist consultations, physiotherapy and speech therapy.
Sagicor’s vice president of group insurance Susan Boyea said the programme would initially involve a specific pool of health and medical providers but it left the door open to medical firms with “the technological capability to deliver a virtual, yet personable doctor-patient experience.”
Boyea said the programme had been accelerated to help flatten the curve during the pandemic and was intended to facilitate access to healthcare services especially for people with chronic medical issues.
Given the high rate of internet and mobile penetration in TT, Sagicor’s initiative could easily form the basis for more widespread adoption of telemedicine across the healthcare industry.
“The scope is limitless,” says Professor Zulaika Ali who pioneered telemedicine in the Caribbean under a 2004 programme which sat in the university’s medical sciences faculty.
Known as UWI Telehealth, the project gave children who had medical problems that couldn’t be diagnosed or treated in TT access to experts attached to the SickKids Foundation in Canada.
Yet despite the programme’s success, there’s been little to no focus on telemedicine in the health ministry over the past decade.
And nothing since the pandemic began, beyond a cursory statement from Minister of Health Terrence Deyalsingh who announced a plan in early April to set up video conferencing facilities at Camp Balandra to facilitate consultations between the patients quarantined there and psychiatrists and psychologists attached to the University of the West Indies.
A spokesperson for the Ministry of Health could not be reached to confirm whether those video consultations had actually started.
But the slow pace of adoption of telemedicine here contrasts sharply with the United States and other developed countries where there has been a massive uptick in demand for HIPAA-compliant telehealth services since the coronavirus outbreak.
In just one US-based example, Teladoc Health, the largest publicly-traded firm in the telehealth sector, reported that its remote medical appointments had more than doubled since early March to around 20,000 a day.
And in the UK, where telemedicine had been held back for years by strict regulations, general practitioners welcomed new policy changes a month ago following which they were told by the National Health Service to switch to remote consultations in a bid to combat covid19.
Up to press time, a number of questions sent to Minister Deyalsingh inquiring about the government’s plan for using telemedicine remained unanswered.
Still, the steps taken by medical professionals like Dr Dolly and Mr Arneaud, and companies like Sagicor appear to show the private sector isn’t prepared to wait.
And it’s not just the big companies.
One startup run by entrepreneurs Shiva Ramsingh and Jenieve Alexander, both graduates of the Arthur Lok Jack Global School of Business, has been working on a local telemedicine app called Treatable since 2018.
According to Ramsingh, the app’s security and privacy features mimic the guidelines contained in HIPAA in a number of important ways including having separate patient and doctor modules and ensuring that only the doctor who is treating a patient can see the patient's records.
Ramsingh believes if Treatable goes mainstream, it could help transform a local health sector in need of change.
Such transformation is also in Dr Dolly’s vision of the future.
“I’ve been in the United States for 10 years before calling it quits and coming back,” says Dolly. “Now that I have returned to Trinidad, I’m all about trying to get that level of healthcare that I saw in the United States here in Trinidad.


Comments
"Coronavirus pandemic brings telemedicine to the fore"