East Indian deaths highest of ‘swine flu’ cases

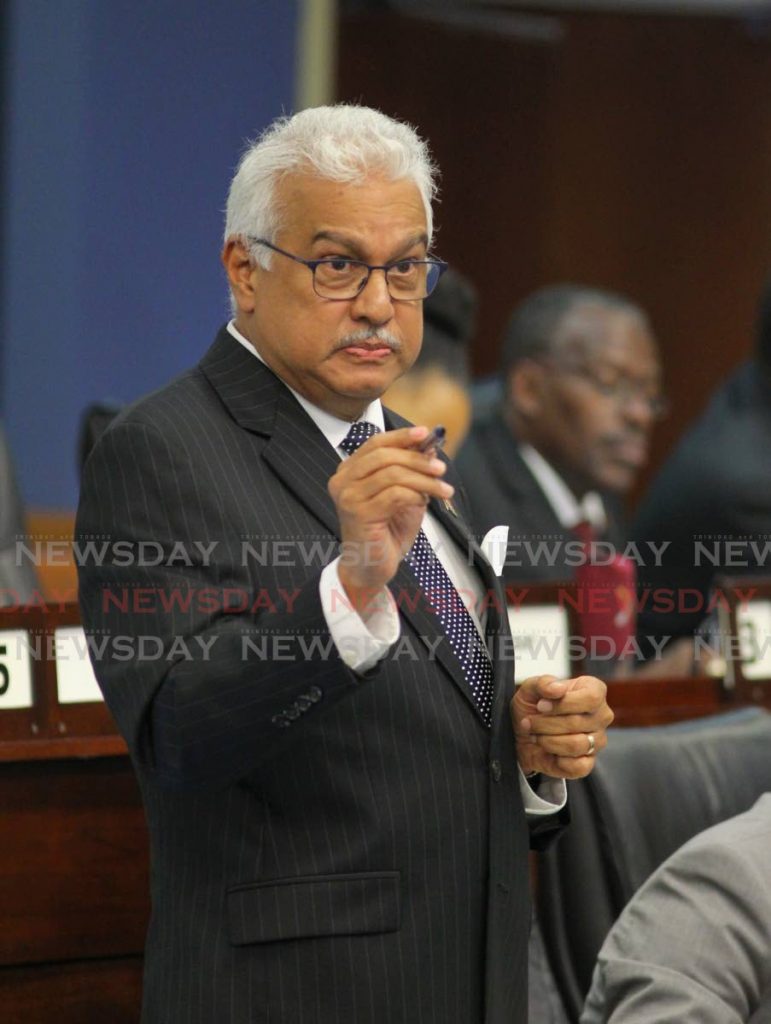
Despite the relatively high number of deaths due to influenza in TT during this flu season, Health Minister Terrence Deyalsingh has stressed that there is no epidemic.
However, due to that number, 32 as of December 6, Deyalsingh has expressed concerns that the flu virus has mutated and is now stronger than medical scientists expected.
He said the number of confirmed influenza deaths for this flu season, October 2019 to May 2020, includes two people from Tobago. He added that there were seven confirmed deaths in 2018 and none in 2017 and 2016. Unfortunately, no records of deaths were kept before 2016.
In a Sunday Newsday interview, Deyalsingh and Chief Medical Officer Dr Roshan Parasram went into detail about the influenza threat.
According to Parasram, at the start of the influenza season in October there were three confirmed deaths. “There was a quick rise in confirmed deaths after that. That’s when we triggered our epidemiology unit to actually look at all the cases individually. So they looked at it in terms of geographic spread, the normal patterns, whether it’s related to risk factors, which we found.”
He said the deaths were related to diabetes, obesity, chronic disease of the lungs and, to some extent, adults over 60. The unit did not find many fatal cases in other high-risk groups such as children aged six months to five years and pregnant women.
Deyalsingh explained the reasons some of these people were at higher risk. He noted that diabetes impaired the immune system which makes it difficult to fight the virus. With hypertension, the body is less able to handle stress. The virus could cause inflammation adding stress to internal organs, and vomiting and diarrhoea make it difficult to keep medication in their systems. Smoking impairs natural lung defence mechanisms which makes the infection worse. And obesity can cause delayed or weakened antiviral responses to influenza as well as poor recovery from the virus.
He added that most deaths were people of East Indian descent from central and south Trinidad. “This is not based on science but we know for a fact that most East Indians live in Central and South. We know for a fact that the incidents of diabetes are highest amongst East Indians. Where do most Indians with diabetes live? Central and South. What the data is showing is that most of the deaths are among the East Indian population living in central and south, and the majority of them were shown to be unvaccinated.”
He stressed that vaccination did not protect people from pneumonia as influenza was not the only cause of the illness. He said he recently had pneumonia and could have died but the test results showed he did not have influenza as he was vaccinated against it.
Parasram agreed saying when people die of pneumonia, others automatically assume they died of the flu. However, the ministry has to wait two to three weeks after a death occurs for test results from labs to confirm influenza because pneumonia has many causes.
Parasram confirmed that the influenza deaths were related to H1N1, the swine flu.
The trivalent vaccines available in TT are effective against the two of 16 subtypes of influenza A – H1N1 and H3N2 – and one subtype of B that is seen in TT.
However, he said viruses tends to mutate. “Once we put pressure on a virus, it’s an organism, it will try to change to survive.
That’s why we have a new flu vaccine every year because it is supposed to cater to changes in the season. So we are looking to see if this particular virus this year, which we suspect because of the larger number of hospital cases and deaths, if it has strengthened in some way.”
He explained that the vaccines are altered every year with the antigenic drift of the virus. Antigenic drifts are small, slow changes that do not change the strength of the virus much. In drifts a pattern of change can be found and predicted. Antigenic shifts are bigger changes that have a greater chance of hospitalisation and death, and a propensity for epidemics.
Deyalsingh went on to illustrate. He said scientists start to formulate the vaccine for the upcoming flu season in January, based on patterns from previous years. “The problem is they are formulating a vaccine to start to give out in October of 2019, ten months in advance, based on their best estimation of what these viruses are going to look like ten months into the future. What happens if their estimate is wrong? It wouldn’t be as effective.”
He said over the last few years, H1N1 went through antigenic drifts, but in 2009 there was an antigenic shift – a rapid, unpredictable change – which caused a pandemic or global epidemic. “So the question needs to be asked, are we seeing some sort of shift that wasn’t catered for in January 2019?”
He said the ministry continually sends samples to the Centers for Disease Control and Prevention in the US which would determine such.
In the meantime, he emphasised the importance of getting vaccinated. To that end the ministry continues with its vaccination drive.
The cumulative number of vaccines administered to the public for this flu season, up to December 6, was 33,101 with an uptake of about 8,000 per week. The ministry purchased 100,000 vaccines, each costing US$2.44, and is already in the process of buying 60,000 more.
Although uptake is higher than last year, the ministry expects an upsurge in influenza cases with the influx of visitors from North America over the Christmas and Carnival seasons. “North America is the basic source of the influenza virus during winter time. They are going to come down here now and spread the virus, so it is imperative that our local population protect themselves and get vaccinated.”
He said ministry personnel were talking to people one-on-one at health centres and distributing vaccines. He said when people with chronic diseases, pregnant women and children go to health centres for their usual visits or treatments, they are approached and offered the vaccine.
He also encouraged people with HIV and those on cancer treatments to get the vaccine once a doctor clears them to do so.
He said it was illegal to go into schools to vaccinate children. “We cannot as a ministry vaccinate children without parental consent. We could be taken to court. That’s why we have to appeal to parents to take the initiative, accept the responsibility for your child, and take your child to either your paediatrician in the private sector or the public sector to be vaccinated.”
Parasram noted that the symptoms of the cold and flu – runny nose, fever, congestion, cough, and body pains – are similar. The difference is in the severity of the symptoms and how long they last.
“It’s very hard for most of the population to tell early on whether they have the flu or the common cold. That’s why we are urging people, especially those in the high-risk groups, to get a physician to look at you early on. If you see a fever persisting more than two or three days or you have vomiting, abdominal pain, diarrhoea, those kinds of severe symptoms, don’t wait to think it’s the common cold. Just go in and get assessed. Better to be safe than it turns out to be the influenza and it’s too late to treat the complications.”
Additionally, he said influenza is highly infectious and is spread by droplets from sneezing and coughing. Any large gathering such as parties or house limes will increase transmission. He advised people to stay away from groups if they are sick, and if children are sick, they should be kept away from school.
“We want to give a nod to principals, teachers, and employers. If people are ill, send them home. Employers, if someone is sick you have to be a little flexible because your whole workforce will go down from one person.”
Deyalsingh gave several suggestions to the general population. These include frequent hand washing, not touching your face with your hands, coughing into your elbow or using tissue or handkerchief, isolating yourself if you have the flu, and seeking medical attention as early as possible.
The endemic channel
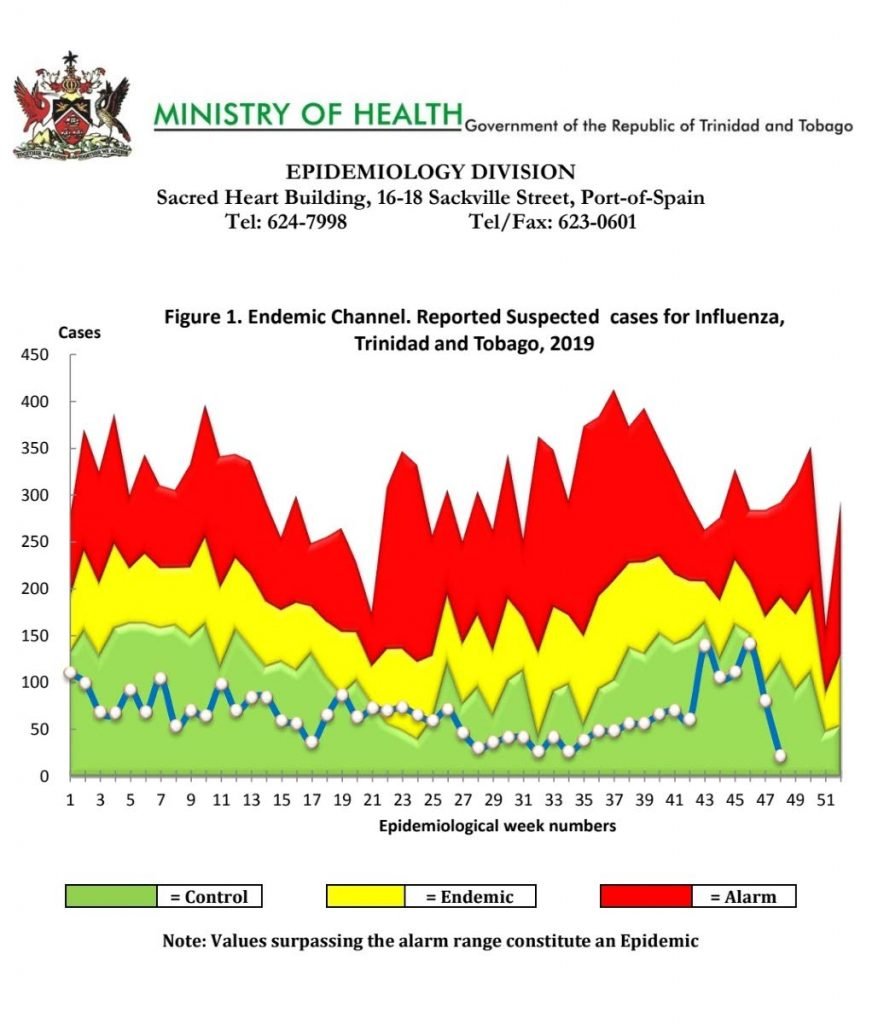
Chief Medical Officer Dr Roshan Parasram explained the number of influenza cases within the expected normal range for TT.
He said the endemic channel is used to determine if there is an epidemic.
He said the Health Ministry gathered data of suspected cases every week over the last five years and calculated the average number. From this, the number of cases for various states were calculated for each week. The states include “in control,” endemic – the expected normal seasonal range, cause for alarm, and epidemic.
He referred to a graph illustrating the endemic channel where the blue line indicates this year’s numbers – week 48 had the lowest number of suspected cases, approximately 20. The highest number was in week 46 with approximately 135. These were both in the “in control” range.
There was an upsurge at the beginning of the flu season between weeks 43 and 46 but there has been a drastic drop since then. The only time this year’s numbers stepped into the “endemic” or normal range was between weeks 21 and 25 where the numbers were less than 75 suspected cases.
Health Minister Terrence Deyalsingh emphasised that the number of suspected influenza cases as of December 6 was 3,232 – the lowest since the number of cases peaked at 7,118 in 2014. He said TT is a few hundred suspected cases under the epidemic line and if there was an epidemic, the 2019 numbers would be above the red area of the graph.


Comments
"East Indian deaths highest of ‘swine flu’ cases"