MORE MENTAL HELP
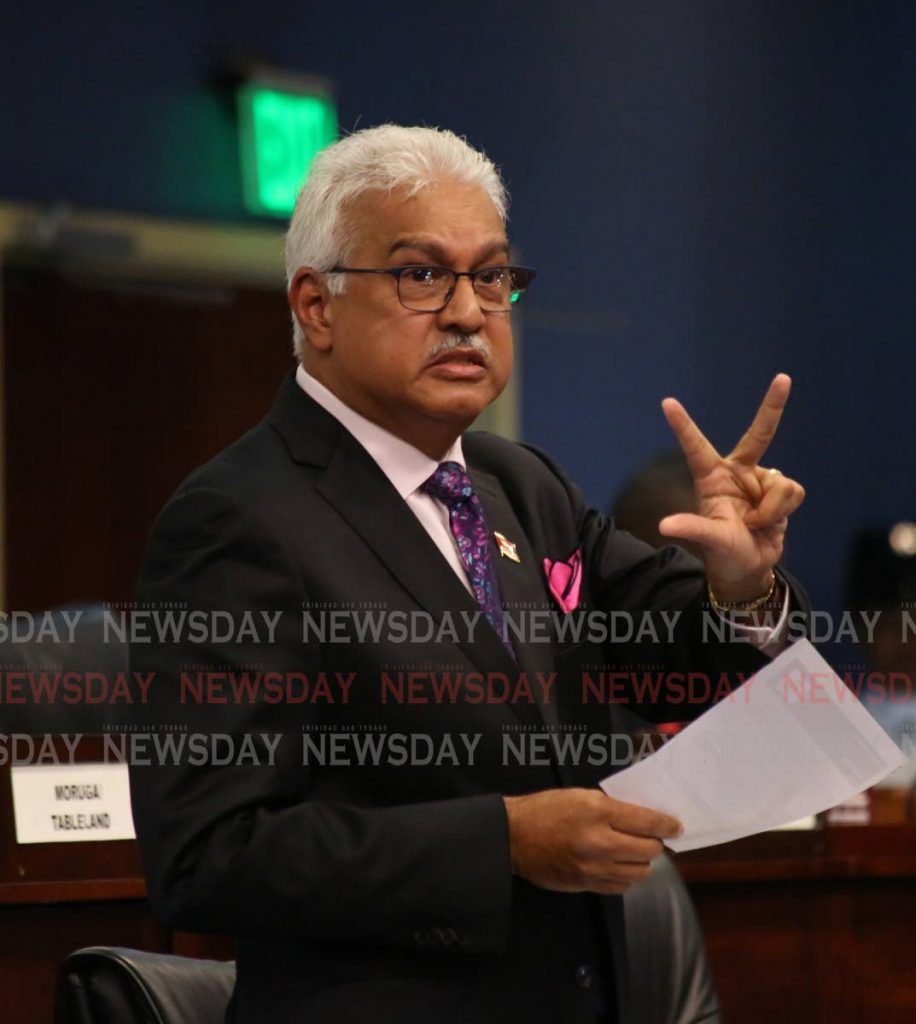
HEALTH Minister Terrence Deyalsingh said a new central mental health facility is to be established, together with supporting satellite facilities.
He was contributing to budget debate in the House yesterday.
He said St Ann's Psychiatric Hospital is 117 years old, and the present model for mental health care is seeking treatment at the end of psychoses and after the disease has progressed.
Deyalsingh said the process of decentralisation had begun and there would be a new, centrally-located, easily accessible, major mental health facility "not tucked away in St Ann's, where people from Cedros and Toco can't reach it." It would be supported by satellite facilities so people can be reintegrated with their families and communities.
He did not say where the new facility would be.
"The big issue in health these days is mental health," he said. "And I am going to tell this country what we've been doing for the past two years so it doesn't seem to be a kneejerk reaction for what happened in...Arouca."
He was referring to the police removing 69 people, some of whom were in cages, from the Transformed Life Ministry in Arouca last week. The incident has sparked a debate about mental health services.
Last week it was also reported that acting CEO of the South West Regional Health Authority (SWRHA) Dr Pravinde Ramoutar told a World Mental Health Day symposium there were more than 16,000 names registered at SWRHA psychiatric clinics.
Deyalsingh said the ministry has concretised a decentralisation plan for mental health which has been talked about since the 1960s. He said the first consultation was held from March 6-10, 2017 with PAHO, and in February 28, 2019 the post of mental health director was approved and the candiate will begin work in November 2019.
"So we have been discussing a new decentralisation plan for mental health two years now and we are ready to rock and roll."
He said with mental health in TT people are caught at the end of their issues and when they have developed to chronicity. He added, like NCDs, mental health issues should be caught as early as humanly possible.
Deyalsingh said this country has a mental health policy for the first time, and as this "new journey" begins, the term could be changed from "mental health" or "psychiatric care" to "behavioural health wellness services."
"That will start with the destigmatisation of mental health."
He said a life-course approach would be adopted for behavioural health.
Deyalsingh said the outcomes of decentralisation would be: increased accessibility across the life-course especially adolescent mental health; increased integration with family and the job market; superior clinical outcomes; and a decrease in stigmatisation.
He also provided suicide statistics from the police Crime and Problem Analysis unit, which showed: 113 suicides for 2013, 104 for 2014, 111 for 2015, 104 for 2016, 103 for 2017, 75 for 2018 and 69 up to September 2019. Deyalsingh said there was a drop of about 25 per cent from 2017 to 2018.
He said with decentralisation of mental health services the three divisions with the majority of suicide cases, Central, Northern and Southern, would get the type of attention they needed.
"So when you have these satellite centres you can catch people earlier."
Deyalsingh also gave a breakdown of public-sector medical staff: 1,783 administrative staff, 5,611 nurses, 149 managers, 1,320 laboratory and technicians, 2,565 support staff, 1,783 doctors, 303 pharmacists and 371 interns. He said the total was 13,884 and if vertical services from the ministry head office were added the total is 17,884, which is 2.8 per cent of the labour force.
"And not one healthcare worker was laid off. And today I want to thank each one for the sterling work that they do."
He said a 2019 PAHO report with statistics from 2017 showed TT had the lowest maternal mortality rates of 21 countries in the non-Latin and Caribbean states and among 38 countries in the Americas, only six countries are doing better than TT. He predicted the 2018-2019 figures will be even better.
"We are recognised around the world as a leader in how to reduce maternal mortality and infant mortality rates."
He said this year there was one maternal death in the public sector, when in years gone by the figure would have been eight.
He also said in the "free healthcare service...which we like to badtalk," the public health sector does 92 per cent of deliveries, or 15,000 out of 16,849, with 27 per cent by caesarean section. Deyalsingh said the cost of a delivery in the private sector for caesarean section was $40,000 and $20,000 for normal delivery. and the 15,000 deliveries would have cost citizens $383,438,400.
"That is what this free healthcare system does."
Deyalsingh said the cost for a premature baby in the neonatal intensive care unit for the minimum stay was $500,000, and if the baby has to stay for months, it goes up to $1 million per child. He questioned which parent without insurance could afford to pay for that.
"But we take this for granted."
He said in healthcare in TT you could do 99 things right, "but if you do one thing wrong you get crucified by the media."
He added: "We are ungrateful."
On the Couva facility, he said the University of the West Indies would incorporate it into a "corridor of medical training excellence" together with Mt Hope and the Penal/Debe Campus. Deyalsingh said this will be anchored by an offshore medical school to train foreigners, which will bring in foreign exchange and medical tourism.



Comments
"MORE MENTAL HELP"