Detecting and treating prostate cancer

SATYENDRA PERSAUD and SHIVAN GOOLCHARAN
Last week we looked at screening for prostate cancer – this week we look at what follows an elevated PSA (Prostate Specific Antigen) reading.
If my PSA is raised what happens next?
If the PSA is not too high, your doctor may simply opt to repeat it as many things may cause a slightly elevated PSA including bicycle riding, infections or even ejaculation. Nowadays, MRI scans are also being used to help with diagnosis. This is not yet widespread in Trinidad but may be worthwhile to discuss with your urologist. If your prostate feels abnormal, your PSA level is worrying or your MRI is abnormal, your doctor will likely suggest a biopsy which should be done by a urologist.
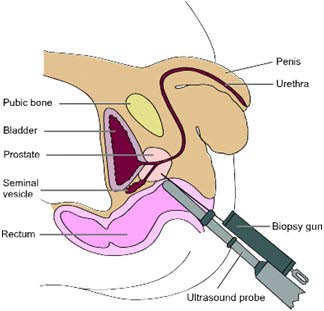
What happens during a prostate biopsy?
A biopsy is done using a small ultrasound probe inserted in the rectum. At least 12 small pieces are taken of the prostate and looked at under a microscope to check whether there is cancer, and if so, how aggressive it is. The biopsy may cause minor discomfort and most men have some blood in the urine for a few days. You may even experience some blood in the semen. These usually clear on their own. There is also a small risk of infection. During a prostate biopsy, several small bites are taken from the prostate. There is minor discomfort only.
If the biopsy is negative, what happens next?
If your biopsy comes back negative, your urologist will have several options. Simply repeating your blood test in a few months is the first one. He/she may also opt for further tests such as an MRI to determine if you need a repeat biopsy.
What if the biopsy is positive?
If this is the case, you may require further testing to see whether the cancer has spread outside the prostate. For this you may require an MRI or bone scan. Newer tests are available that can detect spread better than these traditional tests, but are not available in Trinidad. Before deciding on treatment plans, your urologist will put all of your information together including the aggressiveness of your cancer, your PSA and whether it has spread beyond the prostate. He/she will also take into consideration your life expectancy and of course, your wishes. The aggressiveness of prostate cancer is stated as the Gleason Score and is assigned a score of six-ten with six being the least aggressive and ten the most.
What are treatment options?
If your cancer is confined to the prostate, there are several options:
Active surveillance – this involves keeping a close eye on things with frequent blood tests and even a repeat biopsy. Treatment is only administered if necessary. In this way, the side effects of treatment are delayed for as long as possible. This is only suitable for men with low risk disease.
Radical prostatectomy –The prostate is removed surgically. It can be done via open surgery or using a robot. Side effects include bleeding, rectal injury, erectile dysfunction, incontinence or difficulty passing urine. It is offered as an option to men who are fit for surgery.
Radiation – Radiation may be concentrated on the prostate over a number of weeks or small radioactive seeds may be implanted into the prostate – the latter is called Brachytherapy and is suitable for men in whom the prostate is not too large. Radiation also has side effects including damage to the rectum or bladder and erectile dysfunction.
What if the cancer has spread outside the prostate?
This is called metastasis and in this case your doctor may opt to simply observe you for now if you have other major medical issues and you have no symptoms. More often, your urologist may choose to lower your testosterone either through tablets, injections or a minor surgery on the testicles where the insides are removed. This is done because prostate cancer feeds off testosterone. In some cases chemotherapy may be added to this treatment.
Dr Satyendra Persaud is a lecturer in urology at the University of the West Indies and is responsible for both undergraduate and post graduate teaching. He is a consultant based at the San Fernando General Hospital and is co-ordinator of the Residency Program in Urology. He is a Fellow of the Royal College of Surgeons of England.
Dr Shivan Goolcharan is a urologist in training at the Eric Williams Medical Sciences Complex/University of the West Indies.


Comments
"Detecting and treating prostate cancer"