Doctors need care
PART II
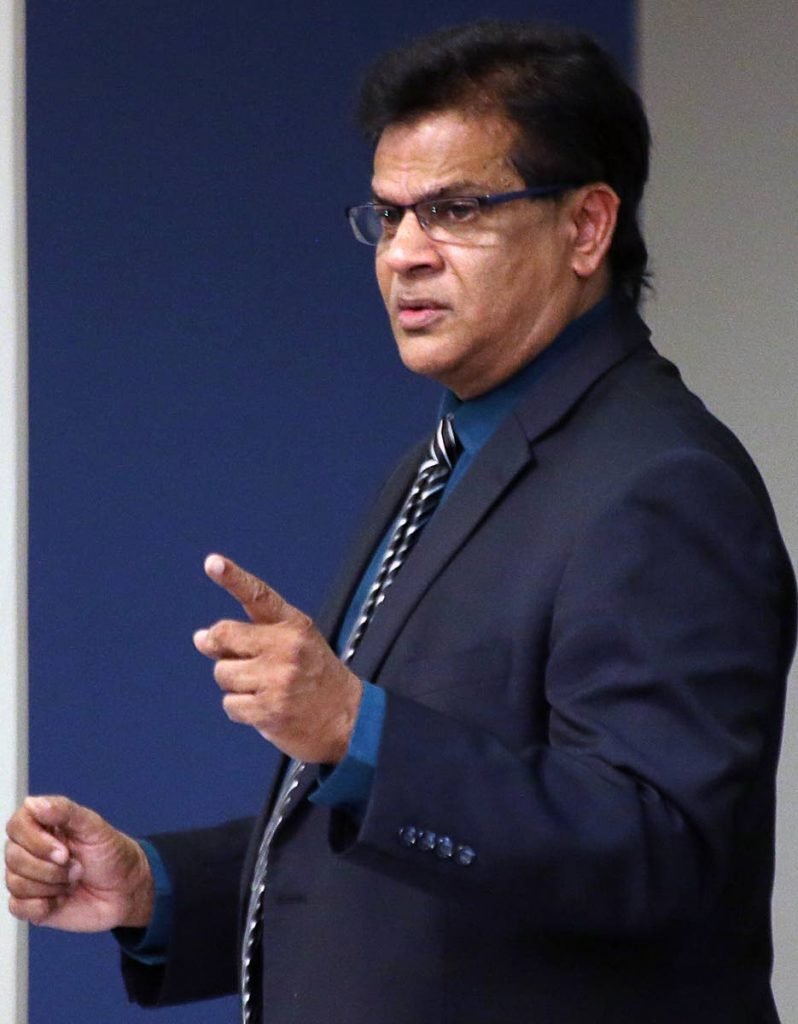
WHILE there are many causes for physician burnout – among them the conditioning of medical education, work-related stress, and a lack of work-life balance – former health minister Dr Fuad Khan believes burnout occurs later on in a doctor’s career.
Khan spoke to Newsday after a young female doctor in the local health system spoke of physician burnout and how it affected her.
For Khan, burnout occurs “in practice, and as you go up the ranks to become a consultant.” He does not believe that younger physicians suffer from burnouts, but that they are tired.
In a phone interview, Khan said all doctors worked very long hours and “it really did not affect you to any great extent. You’re young and you have strength to do it. But physician burnout occurs later down in life.”
He said a lot of doctors eventually realised: “What they were hoping to get and what they have are two different things. But yet they have to continue working, paying litigation fees, paying this, paying that, and at the end of the day, the remuneration is not as great as you thought it was. A doctor only makes money when he sees a patient.
“So he has to keep working indefinitely, and that is the ones who are subject to burnout. And different specialities have different levels of burnout.”
He said burnout in a surgeon is major, while psychiatrists suffer from other types of problems, “not really burnout,” he said.
He also said a lot of local doctors were “doing both public and private practice, and that double action could burn them out.”
Dr Lucy Sand* said while doctors do make a “bit higher salary than the average,” nothing is put in place for their care and well-being especially in the public health institutions, and while there is a certain amount of glamour attached to the profession, “You are pressured to earn extra to afford basic amenities.
“Nothing is put in place for us. Yes, we do make a bit higher salary than the average, but our bills are also higher than the average person. You have to get a good vehicle if you’re working a midnight shift. Given the road conditions in Trinidad, with flooding, etc, more than likely you would want to get an SUV. Then you’re going to have to rent or try to save to build a house. Or buy a house.
“We do not even qualify for Housing Development Corporation (HDC) houses. I think only recently they put us back in the bracket, and then they won’t even see us as first priority,” she said.
She believes while health authorities push quality, “They neglect what the quality would be at our (doctors’) expense. They push quality, but they don’t give us the tools that we need to manage patients properly.”
She has taken to working extra hours to make extra income, with her work day starting at 8 am and ending at 7-9 pm.
Doctors on contract get 21 vacation days, which must be earned within the first year of the contract. A doctor who is permanent, gets 28 vacation days for the year. However, 14 days of casual leave are taken out of that. “If you take 14 casual days, just know that you have seven to 14 vacation days left,” Sand said. The doctors are also only allowed 14 sick days for the year. The TTMA confirmed this, telling Newsday under their contracts doctors receive 14 days’ sick leave, and 21-28 days’ vacation, depending on contract and compensatory days for additional work.
But working long hours is something all doctors had to do. Khan, a urologist, said as a young doctor, he sometimes worked 36 hours straight.
“Nowadays the young doctors do not do that. They have a fixed time, and I think like about 15 hours, and the other eight they can go home. They do not suffer from a burnout like we did in our days,” Khan said.
While some doctors might work 24-hour shifts, he added, “(The) Medical Professionals Association of TT (MPATT) negotiated for them to go home after 16 hours and someone else work the other eight hours.”
Sand had an issue not only with long working hours but also the fact that there are no medical insurance plans for doctors under the health authorities and no mandatory medical checks. The TTMA confirmed this in an e-mail, saying, “There is no medical plan at present in the public healthcare system.”
“However, TTMA is currently working on a group health plan for its membership.
“Doctors, on an individual basis, can seek medical insurance at their convenience. There are no mandatory medical check-ups in the public healthcare system,” the TTMA said.
Khan believes health insurance is not necessary for everyone, since “doctors take care of their own.
“If a doctor comes to you and says there is x, y, z ,you take care of them, and (they) probably get preference in the public healthcare system. Health insurance is not necessary for everyone, as far as I am concerned.”
Sand strongly believes there should be mandatory medical checks.
“I entered medical school with medical requirements. But I entered medicine as a professional without any medical requirements. I was not screened for any diseases; I did no blood tests for my company. I was not required to undergo any tests, including HIV or any of those tests.
“I think it should be mandatory that doctors have health checks, even once a year. Not that we (should) have to pay for it, that it is covered in our contracts or covered within our permanent positions,” she said.
Sand has seen being a doctor exact a heavy price from some of her colleagues.
“I know doctors who smoke, doctors who are alcoholics, I know doctors who are promiscuous...I recently had a colleague who is in rehab right now. He actually collapsed on the job. He presented to work and the nurses had to rush in to him to prevent him from seeing patients, because he was delirious on an overdose on some medication he was taking. That happened just last month or so.”
She sees the lack of medical plans in medicine as “hypocritical.”
“We are not required to see doctors, but we preach and tell everyone they should visit their doctor.”
Similarly, Dr Yansie Rolston, UK-based disability and mental health specialist advisor, in her article on Why Doctors Mental Health Matters, also gave the example of a doctor afflicted by burnout. She spoke of a Dr Naresh* who was diagnosed with cancer while going through a divorce and seeking custody of his children. The pressures of attempting to balance his work and personal life led Naresh to “self-medicate with alcohol, cigarettes, promiscuity, and misused opiate prescription drugs which were easy for him to access. Until one day, after a serious lapse in clinical judgment which endangered the life of a patient, he had to acknowledge the gravity of his mental state, and that his impaired performance could no longer be ignored,” the article said.
Khan believes, however, doctors with addictions “have an underlying addictive personality. It is not the job doing them that.”
Sand sees several solutions, such as having a gym at health institutions, as ways to combat physician burnout. This was also recommended by the TTMA. While saying “employers should recognise that medical employees face high stress,” the association recommended that the doctors’ employers should “provide healthy eating options at the various institutions and incentives for physical activities such as gym access and Employee Assistance Programme (EAP) services at all staff levels; on-call rosters that do not negatively impact on sleep and include reasonable amount of rest time; on-site facilities such as bathroom, lounges and on-call room for short naps.”
Sand was not aware whether or not local doctors had access to EAPs, but the TTMA told Newsday there is one: “Yes, all Ministry of Health personnel and RHA-employed doctors can access an EAP programme facilitated by the Ministry of Health. The process is a confidential one involving contacting the Ministry of Health at 285-9126 ext 2512, where a code is given to the doctor and a number for a service provider. “
It said there were three providers doctors can access and they can also seek assistance from their respective RHAs.
Sand also believes managerial courses should be put in place for consultants, since, “When we hire consultants, they are going just based on academic qualifications and clinical experience...They should train them and screen them.
“We have people who are educated and they don’t know how to pull a shift, how to delegate responsibility.”
The TTMA said extra and appropriate staffing at health institutions would help as well.
The physical, mental and emotional well-being of doctors are important, it said, since “a happy doctor equals a happy patient” and “once doctors are secure then they would be able to function more efficiently in the decision-making and optimal care of their patients.”
For Sand, fixing the problem means fixing the culture.
“It is very hard. We have a workaholic culture where we must do, we must give, we must push and we must fix. And sometimes, you might wake up a day and not feel well, and it – generally through my mind – it goes, if you’re not dying, get up and go.”
But Rolston’s article reminded, “Doctors are fallible human beings and should not have to silently endure feelings of shame, embarrassment and guilt because they are struggling mentally. Stigma, discrimination and misperceptions of mental health affects everyone and needs to be continually challenged.”
*not their real names


Comments
"Doctors need care"