An Aids-free TT

It’s a success story that needs to be told, he said, and he credits six key policy interventions over the last 24 months for the breakthrough.
In November 2015, the National Aids Coordinating Committee (NACC) was moved from the Ministry of Health to the Office of the Prime Minister, giving a greater priority and access to resources.
In May 2016, the country signed on to a UNAids agreement to eliminate the spread of the virus by 2030.
A $7 million investment in Cellma, a health industry software for monitoring patient data.
Negotiating with the US Embassy for access to funds from the President’s Emergency Plan for AIDS Relief (PEPFAR), to the amount of US$250,000, granted to the Medical Research Foundation of TT (MRF) for their Aids clinics.
Changing the supplier of anti-retroviral drugs from a central tender to the PAHO strategic fund, resulting in an annual savings of $70 million.

Nine million dollars allocated every year for five years, approved by Cabinet, for viral load testing machines.
“Regardless of your status, regardless of your viral-load count, we are now going to treat everybody once you have been deemed to be HIV positive,” Deyalsingh said.
Government provides free clinics, counselling—and most importantly—free anti-retroviral drugs to anyone diagnosed with the disease. The Health Ministry estimates that there are 11,000 people infected with HIV in TT.
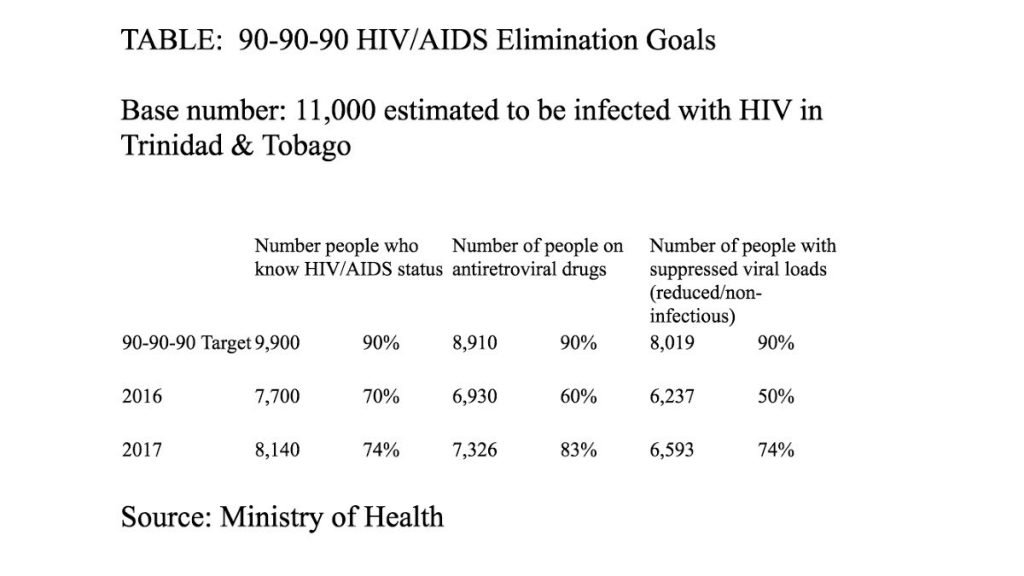
As part of the UNAids pact, TT has also agreed to a 90-90-90 goal, where by 2020, 90 per cent of those infected should know their status; 90 per cent of that number should be put on antiretroviral drugs; and 90 per cent of that should have their viral loads suppressed.
Since receiving the mandate, the ministry, the NACC and other NGOs like the MRF have stepped up their education and outreach programme to get more people tested and registered in the system. While still some way away from the target, in one year the number of people who know their status is up four percent from 2016 to 2017, the number of people on antiretroviral drugs is up 23 per cent, and the number with suppressed viral loads is up 24 per cent. (See table)
“The figures speak for themselves. You can’t argue with figures, you can’t argue with success. That speaks volume for the government’s policy position. We have been able to bring back people who have fallen off,” Deyalsingh said.
However, the ministry is seeking to find 1,700 people who are HIV positive and do not know and will use a public health HIV-Aids awareness campaign for Carnival in its programme to locate infected people and get them treated, Deyalsingh noted over Christmas. This data is determined by a UNAids simulation programme which matches the number of known cases against characteristics of a country to determine the probable number of people who may be infected. He also said there will also be a closer review of the cases of men over 60 and girls who are positive.
The minister acknowledged some of the criticism against him, but remained adamant that Government’s policy is not to support risky behaviour.
In 2016, at the same UNAids signing ceremony, Deyalsingh had been quoted as saying Government would not introduce Pre-exposure Prophylaxis (PrEP)—drugs that allow people who may be at high risk for exposure to the virus to reduce their chances of contraction—as a subsidised form of HIV medication.
Deyalsingh told Business Day Government was not going to spend money on HIV drugs on people who engage in risky behaviour. Asked if this was counter-intuitive since the duty of a government should be too look after the best interest of the population, he said it was Government’s position to provide HIV drugs for those who knew their status.
Dr Ayanna Sebro, a member of the NACC, added that prevention is a comprehensive issue, and any policy should look to strengthening overall prevention, not singling out PrEP. PrEP is only one option, but the outcome may not be what the population expects. Increasing the number of people on antiretroviral medication, she noted, as a method of intervention could address some of the issues people have with PrEP, since regular use of anti-retrovirals can suppress viral loads and significantly reduce the risk of transmission.

Dr Jeffrey Edwards, director of the MRF, estimated that 79,000 people come out to get tested for HIV annually, many of whom are re-testers, mostly during campaigns. There are over 64 testing sites all over the country. Edwards admitted that there was no formal programme in place for monitoring sex workers, since their trade is illegal, but surveys of the community suggest that there are actually low rates of infection among them.
There are also marginalised communities where HIV/Aids may be disproportionately represented, like among homosexual men and transgender people. Poverty also exacerbates the struggle.
MRF has been using PEPFAR funds to help mitigate the fallout from shame, self-hate and fear. The clinics are open at times that are more accommodating and comfortable for its patients. There are also trained peer counsellors, mental health practitioners and “tracers” who call patients who may have fallen by the wayside and encourage them to come back. The clinic has about 8,000 registered patients, but 6,250 active follow-ups. That figure is improving with the tracers’ intervention.
Edwards said among the main reasons given for patients not following up were that they were too poor to afford taxi fare, nor could they afford food. Some PEPFAR funds are used to buy bus tickets, and meal supplements, because the drugs need to be taken on a full stomach.
“We are seeing spectacular increases since we’ve started this,” Edwards said.
The first Aids case in TT was discovered in 1983, two years after the virus, which had been ravaging gay male communities in the United States was isolated and the disease named. Edwards said the strain of HIV in TT is similar to the North American version. And while the disease may have started out in the men who have sex with men category, it is now a heterosexual disease here.
Children have thus been unfortunate victims of the disease, but there is much success. A major achievement by the country has been the near elimination of mother to child transmission of HIV, with a rate of less than two per cent. TT is working towards getting similar certification to Cuba, which was the first country validated by the World Health Organisation to eliminate mother to child HIV infections.
“The mother to child transmission programme, which is very well integrated into the primary care programme and the women’s health programme, is one of our biggest success stories,” Edwards said.

The number of children (mainly adolescents) is about 200, Edwards said, and MRF has a special clinic, also using PEPFAR funds, to provide counselling and support for them.
The mission then, is to educate people about safe sexual practices. In Trinidad, the peak season for risky sexual behaviour is Carnival. In Tobago, it is year-round, Deyalsingh said.
“You want to mitigate risky behaviour but at the same time it’s such a taboo to talk about that even when you try to make interventions, you get backlash. How do you work around that? It might be clichéd but it boils down to personal responsibility,” Deyalsingh said, adding that Government will continue to educate.
There needs to be a significant amount of social research before any sort of targeted intervention is implemented, chief medical officer Dr Roshan Parasram said.
He noted the backlash faced by the ministry after a pilot programme to introduce condoms in schools was criticised for encouraging risky behaviour.
“You have to understand what makes people go toward sexual behaviour, understand the actual core values and the core behaviours that contribute to it, and then mitigate against it in your plans.”
The stigma of HIV/Aids, prevalent throughout the society, is not lost on Government—but neither is the fact that with proper treatment, a disease that was once a death sentence can be controlled, and its victims granted a reprieve to live a longer life.
“We are looking at in terms of being able to de-stigmatise HIV a little bit more but also, just to kind of get people thinking about stigma and what they can do around stigma, so that people would know what HIV is and how it is transmitted, and that you can’t get HIV by touching someone,” Deyalsingh said.


Comments
"An Aids-free TT"